Asked by Pamela Smith on Sep 27, 2024
A nurse developed the following discharge summary sheet. Which critical information should the nurse add? 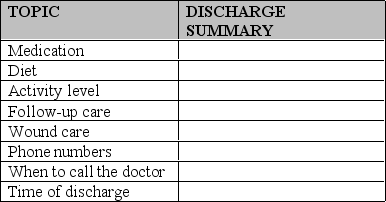
A) Clinical decision support system
B) Admission nursing history
C) Mode of transportation
D) SOAP notes
Discharge Summary
A document containing important information about a patient's hospital stay and instructions for care after leaving the hospital.
Clinical Decision Support System
A health information technology system that is designed to provide physicians and other health professionals with clinical decision-making support as they provide care to patients.
SOAP Notes
A method of documentation employed by health care providers to write out notes in a patient's chart, including Subjective, Objective, Assessment, and Plan sections.
- Understand the purpose and process of discharge planning and patient education.

Learning Objectives
- Understand the purpose and process of discharge planning and patient education.